CRISPR, No Cuts
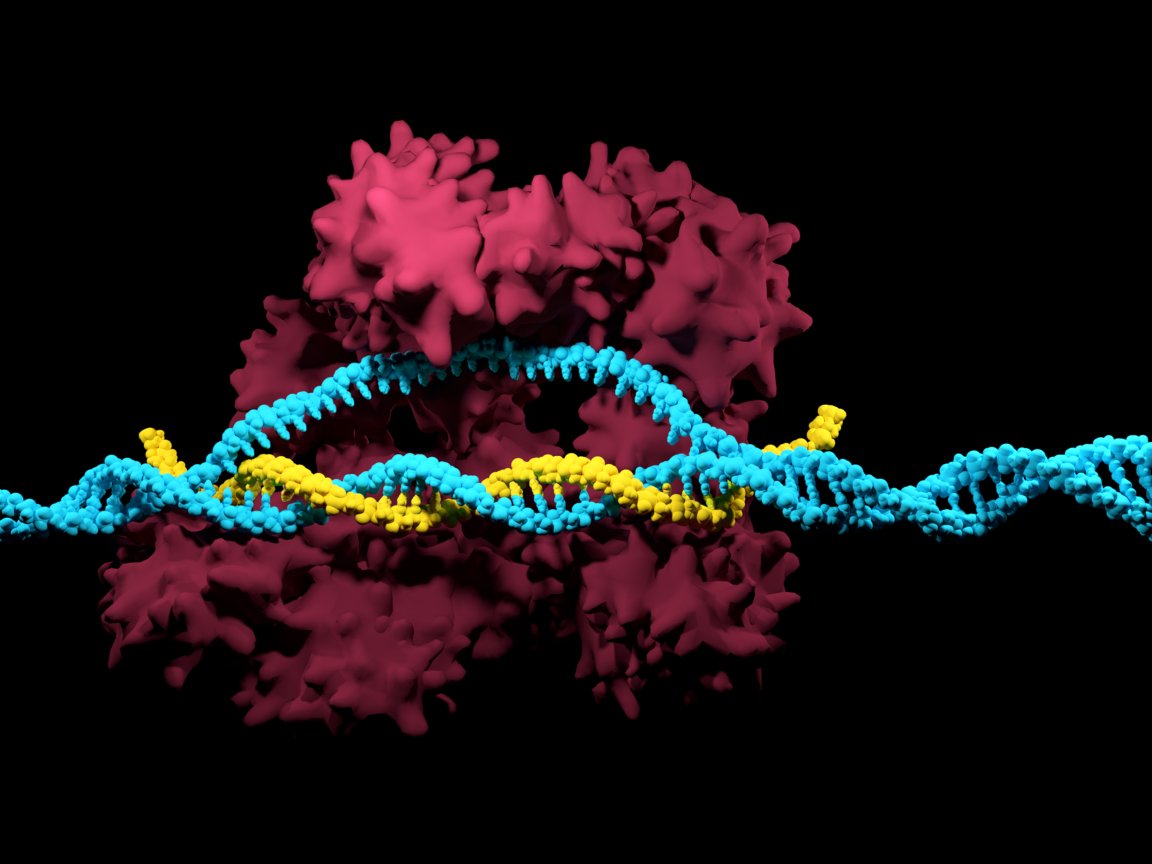
CRISPR-Cas9 technology allows scientists to insert or remove genes by making a cut in a DNA molecule; an ability that has applications ranging from the creation of pigs with lower levels of body fat to the eradication of certain diseases. However, the technique also has the potential to create genetic mutations that may produce undesired side effects.
With that in mind, a team of researchers set out to develop a take on CRISPR-Cas9 technology that wouldn’t require the DNA to be cut at all. A trial of their technique was successfully used on mice to treat several diseases. The study proves, for the first time, that the phenotype of an animal can be altered via epigenetic editing while ensuring the integrity of the DNA is preserved and no mutations are introduced.

“Cutting DNA opens the door to introducing new mutations,” said senior author Juan Carlos Izpisua Belmonte in a press release. “That is something that is going to stay with us with CRISPR or any other tool we develop that cuts DNA. It is a major bottleneck in the field of genetics – the possibility that the cell after the DNA is cut may introduce harmful mistakes.”
Manipulation Machinery
The technique uses two adeno-associated viruses (AAV) to introduce genetic manipulation machinery to cells in post-natal mice. One contains the gene for the Cas9 enzyme, and the other contains a transcriptional activator and is outfitted with a short single guide RNA (sgRNA) which determines the exact position the enzyme needs to bind to within the mouse genome. Since the sgRNA is only comprised of fourteen or fifteen nucleotides, compared to the twenty that are used in most CRISPR-Cas9 procedures, no cut is required.
When this complex is placed near the DNA set to be modified, it promotes the expression of a particular gene. The same basic principle could be implemented to activate almost any gene or genetic pathway without the potential for unwanted mutations.
In tests using a mouse model of acute kidney disease, the technique was seen to activate damaged or silenced genes, allowing the kidney to function normally. It proved useful for helping liver cells regain the ability to produce insulin, which contributed to a mouse’s recovery from type 1 diabetes.
The team also demonstrated the capacity to recover muscle growth and function in mouse models of muscular dystrophy, a condition that’s linked to a gene mutation. But instead of seeking to correct it, the expression of genes in the same pathway was actually increased — which then took precedence over the mutation.
“We are not fixing the gene; the mutation is still there,” said Belmonte, “Instead, we are working on the epigenome and the mice recover the expression of other genes in the same pathway. That is enough to recover the muscle function of these mutant mice.”
From Mice to Humans
Based on these early trials the method doesn’t seem to produce any precarious side effects, but before any clinical testing gets underway, the researchers will carry out further studies to assess safety, practicality, and efficiency.
Researchers hope the technique could lend itself to developing treatments for a wide variety of neurological disorders, including Alzheimer’s and Parkinson’s disease, by spawning healthy neurons in the same way that it addressed kidney disease in mice. That said, there’s still a long way to go before the technique could be tested in humans.
“There are still multiple steps that need to be examined before applying this method in human patients,” co-first author Hsin-Kai Liao told Futurism. “For example, it must be determined whether host immune responses against the AAV-CRISPR/Cas9 Target Gene Activation system arise in mice or large animals. Safety and ethical considerations will also have to be addressed before bringing this technique to human patients.”
The potential for a safe, efficient method of addressing ailments ranging from Parkinson’s disease to muscular dystrophy is certainly very compelling, but early successes while testing on mice don’t necessarily mean that the technique will be viable for humans. Once the questions pertaining to host immune responses and ethical considerations have been addressed, the team hopes to have a clearer timeline regarding clinical trials.