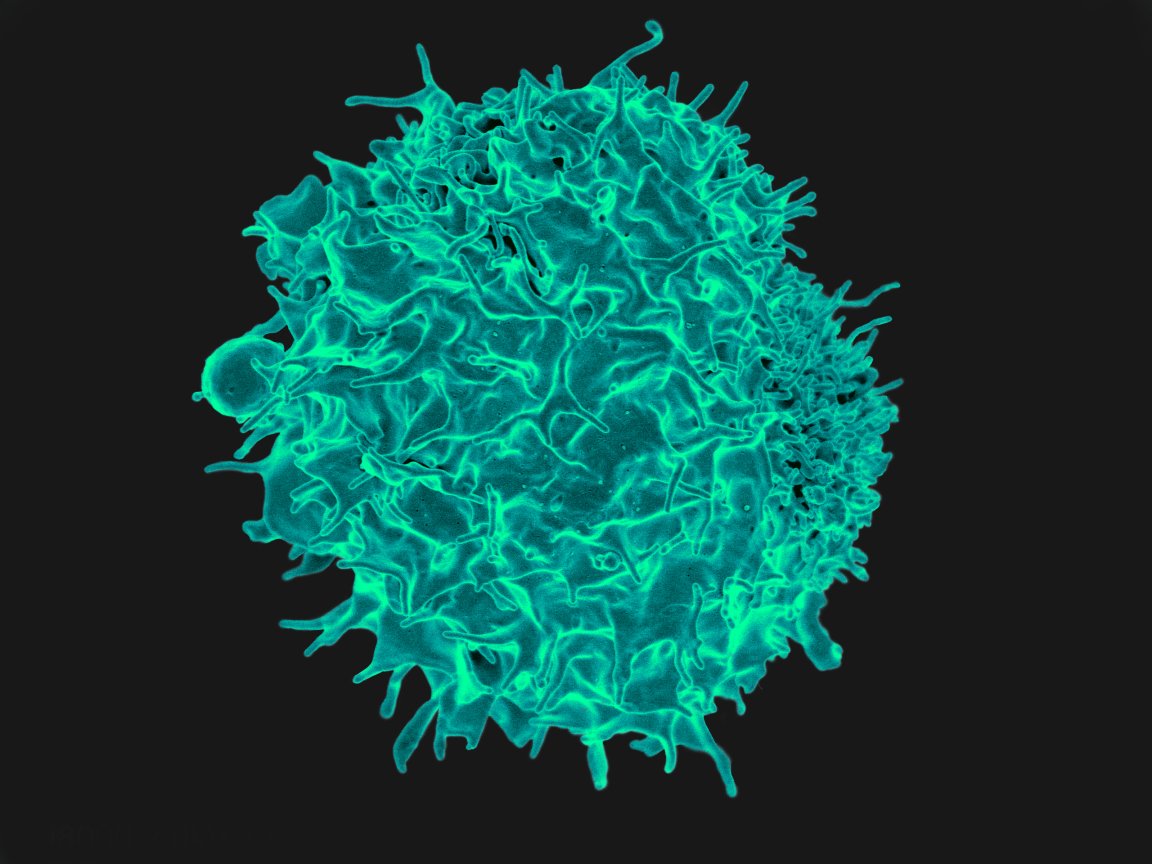
Using T-Cells to Fight Back
One of the first line treatments for cancer is chemotherapy, which can be a long, stressful process. While some patients certainly benefit from the treatment and see their cancer go into remission, others may not see the same effect. For those chemotherapy has failed, as well as others for whom other treatments were unsuccessful, the recent publishing of two new CAR-T studies may provide some hope.
The first, called ZUMA-1, details the results of a clinical trial that treated patients who had certain types of large B-cell lymphoma. The patients had failed to responded to, or had relapsed after undergoing, at least two other treatments.
Led by Sattva Neelapu, MD, of the MD Anderson Cancer Center, and Frederick Locke, MD, of the H. Lee Moffitt Cancer Center and Research Institute, the treatment involved genetically modifying a patient’s white blood cells/T-cells to attack cancer cells. The Food and Drug Administration (FDA) approved the use of such treatments in August, saying it’s “committed to helping expedite the development and review of groundbreaking treatments that have the potential to be life-saving.”

111 people across 22 institutions took part in the study and were treated with axi-cel (later renamed to Yescarta). Of those, 82 percent were somewhat responsive to the treatment, while 54 percent experienced a complete response. 42 percent were in remission 15 months after treatment was administered, and some were still cancer free 24 months after treatment.
“With the FDA’s recent approval of this therapy, we believe this is a major advance in the treatment of patients with relapsed or refractory large B-cell lymphoma and is likely to save or prolong lives of many patients,” said Neelapu. “This study demonstrated that axi-cel provides remarkable improvement in outcomes over existing therapies for these patients who have no curative options.”
The second study also utilized modified T-cells to combat cancer cells. The study treated 28 of its 38 patients with CTL019 cells between 2014 and 2016. Complete remission occurred in 6 of 14 patients with large B-cell lymphoma and 10 of 14 patients with follicular lymphoma. As of 2017, all patients in complete remission after 6 months have remained in remission.
Adverse Reactions
There are some side effects to Yescarta, however. According to the study, 95 percent of patients who received the therapy had severe side effects including fever, lower white blood cell and blood platelet counts, and anemia. 64 percent of patients experienced neurological events, including encephalopathy, general confusion and difficulty speaking. While those symptoms were troubling, they typically resolved within two weeks.
Patrick Stiff, MD, director of Loyola’s Cardinal Bernardin Cancer Center (one of the institutions that participated in the study) explained that Loyola would begin offering Yescarta in 2018, but only to patients who are specifically selected and have had the pros and cons fully detailed to them.
“We are taking a very measured approach to this new therapy, which is effective, but also potentially toxic,” said Dr. Stiff. “The therapy should not be considered a cure-all, since some of the patients did relapse after the therapy.”

Side effects were also present in the CTL019 study: 5 patients experienced severe cytokine-release syndrome, and another 3 suffered from encephalopathy. Encouragingly, the study did note that “no deaths from cytokine-release syndrome occurred.”
Modifying the body’s own cells to address cancer seems to be the way to go when it comes to potential cancer treatments, and it doesn’t just stop with immune cells. In November, researchers from ETH Zurich and the University of Tokyo developed a way to use nonimmune cells for the same purposes — though it’s still a long way from being used to treat human patients.
That said, the future of cancer treatment research looks bright, despite the risky side effects. Of course, given the potential for serious side effects, these treatments are only being used as a last resort. Hopefully it’s only a matter of time before we find an effective treatment that doesn’t come with additional baggage.