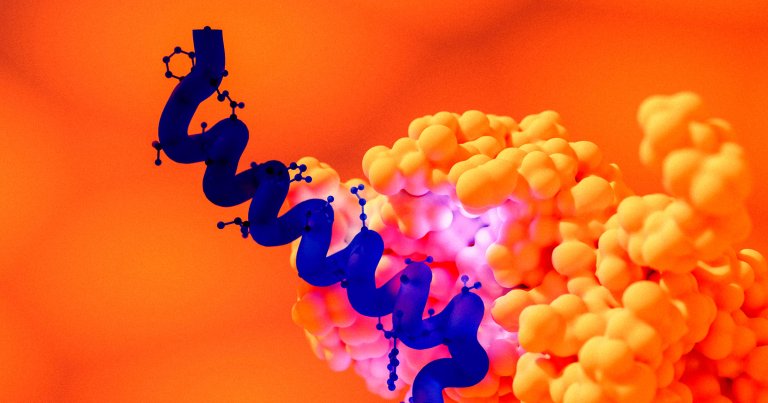
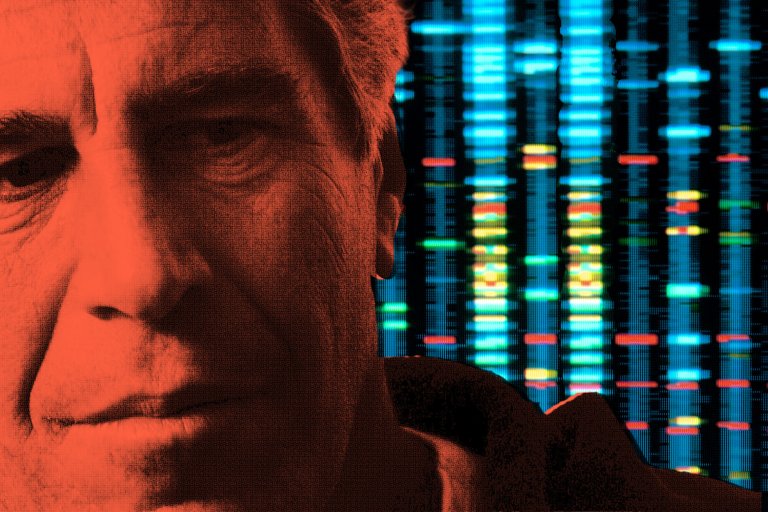
Health & Medicine
Human history has been marked by an unending struggle against bacteria and disease, but each day brings us new research, getting us closer and closer to the cures. Here, we’ll track the latest health and medical research as well as current events that transform our understanding of the human body and, ultimately, saving lives.