When Three People Make a Baby
The long-held belief that we get half our genes from our father and the other half from our mother may not be as accurate as we once thought. In fact, scientists have discovered that your mother’s genes might actually have a few inches on that of your father’s in the genetic tug-of-war involving your genetic makeup.
The culprit is the mitochondria, which, thanks to memes, we all know is the “powerhouse of the cell” — but the mitochondria is much more than that when it comes to fertilization. Sometimes, in the case of genetic diseases, its function can be deadly. But thanks to pioneer physician John Zhang and his team, families with a known history of genetic diseases may have the opportunity to raise a healthy child through the conception of a 3-parent-baby.

Zhang’s team has provided more details about a healthy conception they helped bring about in a paper published on 3 April in Reproductive Biomedicine Online. Zhang used mitochondrial replacement therapy (MRT) to help a 36-year-old woman to conceive a child. While the woman is asymptomatic of Leigh syndrome, she had already had four pregnancy losses, and her family history was marked with the disease. Leigh syndrome is a severe neurobiological disorder that impairs the central nervous system and becomes apparent in the first year of life, often leading to death several years later.
Twenty percent of all Leigh syndrome cases are linked to mitochondrial inheritance from the mother, which is why Zhang’s method of collecting donor immature egg cells (from the “third” person) is proving to be an effective . In his case study, Zhang’s team collected 28 healthy donor immature egg cells and verified if the mtDNA (mitochondrial ) was safe from pathogenic mutations for insertion. A doctor collected 29 eggs from the mother, but only five were suitable for the procedure.
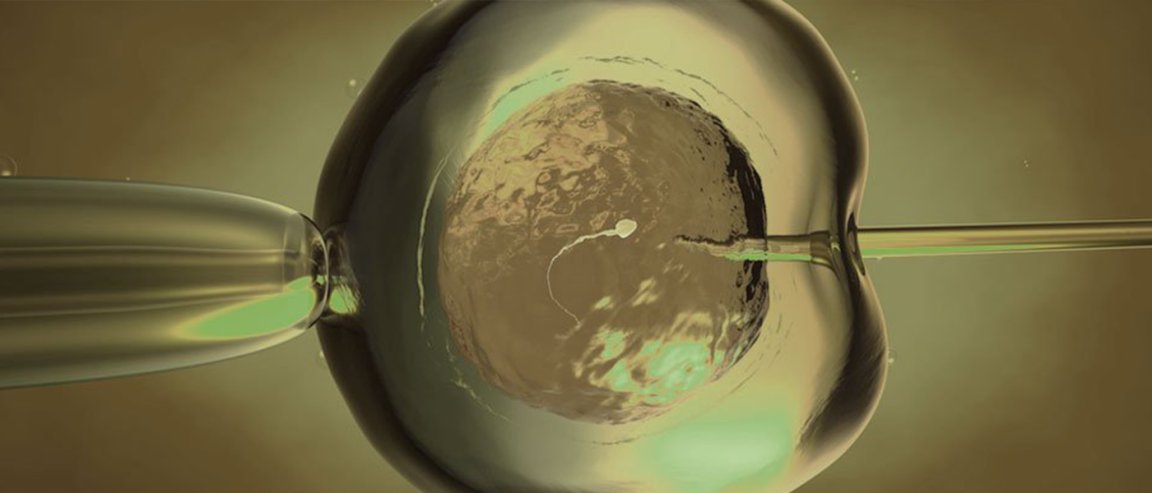
Using an electrofusion technique, which combines different cells with an electric current, the team transferred the mother’s into a donated egg with healthy mitochondria. The hybrid egg was then fertilized by the father’s sperm and transferred to the mother’s womb.
The Politics of Gene Therapy
The MRT technique proved successful with the birth of a healthy male child in 2016. While 25 percent of the mother’s total mitochondria was affected by Leigh syndrome, the disease affected only two to nine percent of the child’s mitochondria.
In accordance with current U.S. federal law, the fertilized egg with the mother’s genome and donor’s cytoplasm was implanted in the mother in a fertility clinic in Mexico. The previous procedures, including egg collection, mitochondrial replacement, and fertilization, were conducted in a private fertility clinic in New York.
While the U.K. leads the world in providing MRT, the U.S. has a difficult history with the technique. As of last year, the FDA greenlighted MRT with male embryos only. This is because any family history of mitochondrial disease would end with the male, as he cannot significantly pass on harmful mitochondrial DNA to any of his potential offspring. Even with the FDA’s approval, the 2016 congressional budget prohibits the implantation of modified embryos into any woman, which is why Zhang’s team went to Mexico.
While many are terrified that MRT will evolve into eugenics and designer babies, it’s obvious that without MRT, Zhang’s patient may have never had her little boy.