
Heart Surgery, Now And Then
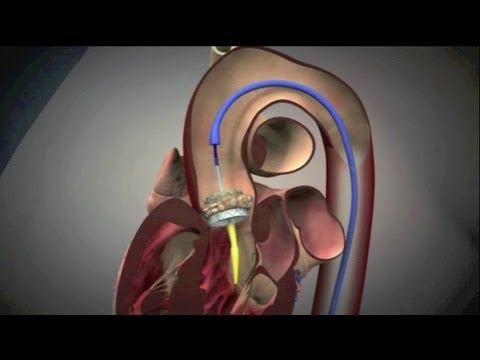
Currently, on the cutting edge of heart surgery is a small implant called the transcatheter aortic valve implantation (TAVI), one version of which is made of bovine pericardium (a tough membrane that surrounds the heart of a cow) encased in a collapsible metal stent. It is designed to clear impaired aortas by being inflated like a miniature expanding doughnut, after reaching it desired position using a previously inserted guide-wire.
While, in most countries, the most common procedure used to treat heart conditions like aortic stenosis (a narrowed valve) is open-heart surgery, the £20,000 (around $25,000) cost of TAVI means that only patients with severe complications that make surgery impossible are treated with the device. Remarkably, doctor’s are now even capable of implanting TAVI in unborn babies. The procedure was first performed on Angela and Jay VanDerwerken’s unborn baby girl at Brigham and Women’s Hospital in 2005 by Wayne Tworetzky, the director of fetal cardiology at Boston Children’s Hospital. The fetus had hypoplastic left heart syndrome (HLHS), which causes the left side to develop improperly — doctors have to create and retain a hole between the left and right ventricles in order to oxygenate the blood sufficiently. This improvement could reduce the rates of miscarriage and infant deaths.
Many think, however, that the future of treatment for heart-related conditions is the artificial heart, which scientists are trying to develop in three main ways:
First, a robotic heart could be created, which would contain tiny rotary motors suspended magnetically so as to assuage the damage caused by friction. And, while several companies are trying to develop them, most notable is Carmat which has been working with world-renowned heart surgeon Alain Carpentier. So far, no models have been tested in animals.

Second, this could be achieved by appropriating a heart. This process involves decellularizing (isolating the extracellular matrix by ridding the target of cells) a heart, modifying it to human specifications, and then encouraging human heart cells to grow around the skeleton heart. In a 2008 experiment overseen by Doris Taylor, now Director of the Center for Cell and Organ Biotechnology at the Texas Heart Institute, scientists were successful in generating electrical electricity but no contraction or pumping motions.
Third, an artificial heart could be created by using 3D printing. This process works almost identically as the one above, but uses a heart printed with amenable materials.
Donors And Antidotes
Due to the TAVI, the rate of heart complication survival is increasing, and surgery is becoming easier to overcome. Thomas Morris reported in The Guardian that, “Just minutes after being given a new heart valve, the patient raised an arm from under the drapes and shook the cardiologist’s hand warmly.” However, due to their high cost and the shortage of donors — the waiting list has doubled in the last 5 years in the U.K alone. Artificial hearts could eliminate the issue of a lack of donors, saving countless lives in the process.
Despite these incredible developments, the most cost-effective and life ensuring way to combat heart disease is to detect it early. Fortunately, major advances are being made in preventive heart treatments, including a silicon sleeve that can help your heart beat and an artificial intelligence (AI) that can predict heart attacks.