Combining New Technologies
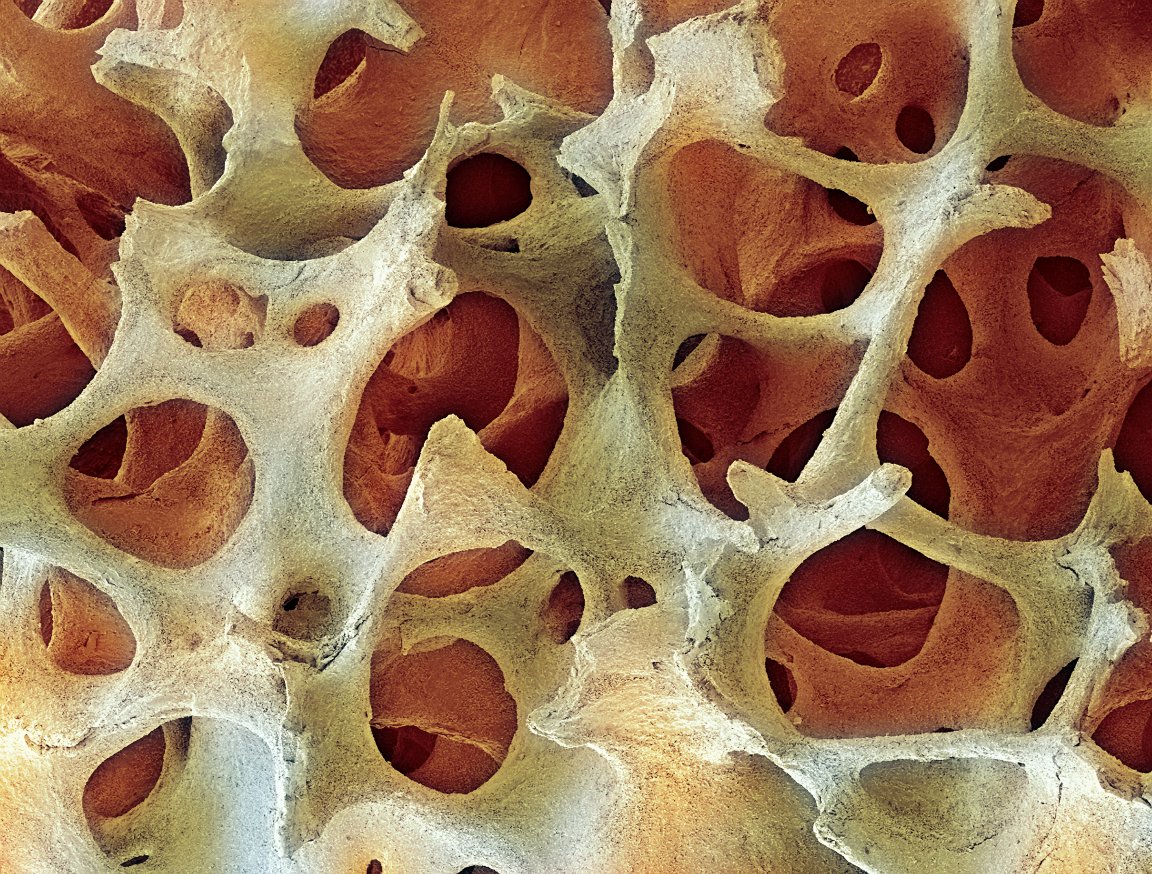
A research team from Northwestern University and the University of Chicago just repaired a hole in the skull of a mouse by regrowing “quality bone.” This breakthrough could render bone-grafting techniques obsolete, drastically improving the outcomes of people with severe skull or facial bone trauma. The technique regenerated the skull bone and the blood vessels it needed for its support in only the injured area more rapidly than past methods and without developing scar tissue.
The researchers achieved a successful result in their experiment by combining technologies. First, they harvested the mouse’s skull cells and then engineered them to produce a potent bone growth-promoting protein: BMP9. They next used a hydrogel created by biomedical engineering professor and research team member Guillermo Ameer as a kind of temporary scaffolding. With this in place, the harvested cells were delivered and remained contained within the affected area.

The skulls of the mice in the study didn’t reject the cells because they were harvested from their own bodies. BMP9 was the chosen protein because it not only promotes the rapid growth of bone cells, but also improves the creation of blood vessels in the surrounding area, which is essential to support healthy bone tissue.
This research demonstrates the possibilities of safe in vivo bone regrowth, a process that is far faster than growing bone outside of the body. It would also be fairly easy for other doctors to adopt, according to Ameer: “[The process is] surgeon friendly, if you will, and not too complicated to scale up for the patients.”
Success on Multiple Fronts
Defects and injuries in the facial bones or skull are very challenging to treat. They often require doctors to graft bone from elsewhere in the patient’s body, such as their ribs or pelvis. Not only is that process painful for the patient, it can be difficult for the surgeon if the injured area is large or if the graft must be contoured to the cranial curve or the angle of the jaw. However, if this new approach proves workable, that process may become a thing of the past.

The technique demonstrated in this research was successful in several key ways. The regenerated bone was higher quality than the bone created using other techniques; the scaffolding confined the bone growth to a specific area effectively; the healing process was faster than that observed following other techniques; and areas of old and new bone were continuous and uninterrupted by scar tissue. All of these results suggest tremendous potential for the treatment of people suffering from aggressive cancers attacking the face or skull or victims of car accidents or other serious traumas to the head and face.
While Ameer did caution that the technology remains years away from potential application in humans, he also noted that the team is optimistic: “We did show proof of concept that we can heal large defects in the skull that would normally not heal on their own using a protein, cells, and a new material that come together in a completely new way. Our team is very excited about these findings and the future of reconstructive surgery.”