When the HIV outbreak first began, most individuals developed AIDS within 8 to 10 years, and once a person was diagnosed with AIDS, they had a two-year life expectancy. It was a death sentence; however, thanks to advancements made in the sciences, that has dramatically changed. In fact, “HIV is no longer a terminal illness.”
This information comes from Kristen Lanphear, a woman who has devoted her life to assisting in the fight against HIV and AIDS.
At just 14 years old, Kristen started working as an HIV prevention educator for the American Red Cross. Since then, she has worked as a prevention specialist at legacy AIDS Rochester, and she currently works as a manager in Community Health Initiatives at Trillium Health, an organization that specializes in providing comprehensive care to those living with HIV or AIDS.
The importance of Kristen’s work cannot be overstated, as HIV is an epidemic that has been plaguing humanity for over three decades, and to date, it has claimed an estimated 39 million lives.
According to the World Health Organization (WHO), in 2013, there were approximately 35 million people around the globe who were living with HIV or AIDS. Of these, some 3.2 million were children under the age of 15. These numbers are dire, especially when one considers that, in previous decades, a great majority of these individuals would have been dead by the decade’s close.
But not anymore.
Thanks to advancements in modern medicine, HIV is no longer considered a terminal illness; rather, scientists list it as “chronic, manageable illness.” It’s not fun, and you will have to deal with it for the rest of your life, but (and this is the notable thing) we can deal with it. We can manage it. And in the end, individuals who have HIV ultimately have the exact same life expectancy as those without the virus.
I recently sat down with Kristen to talk about the amazing breakthroughs that got us to where we are today, and where the fight against HIV may lead us next (Note: This is a rather long piece. If you want information about the history, prevention, treatment, or cure, scroll to the relevant heading).
But First, the Basics of HIV & AIDS:
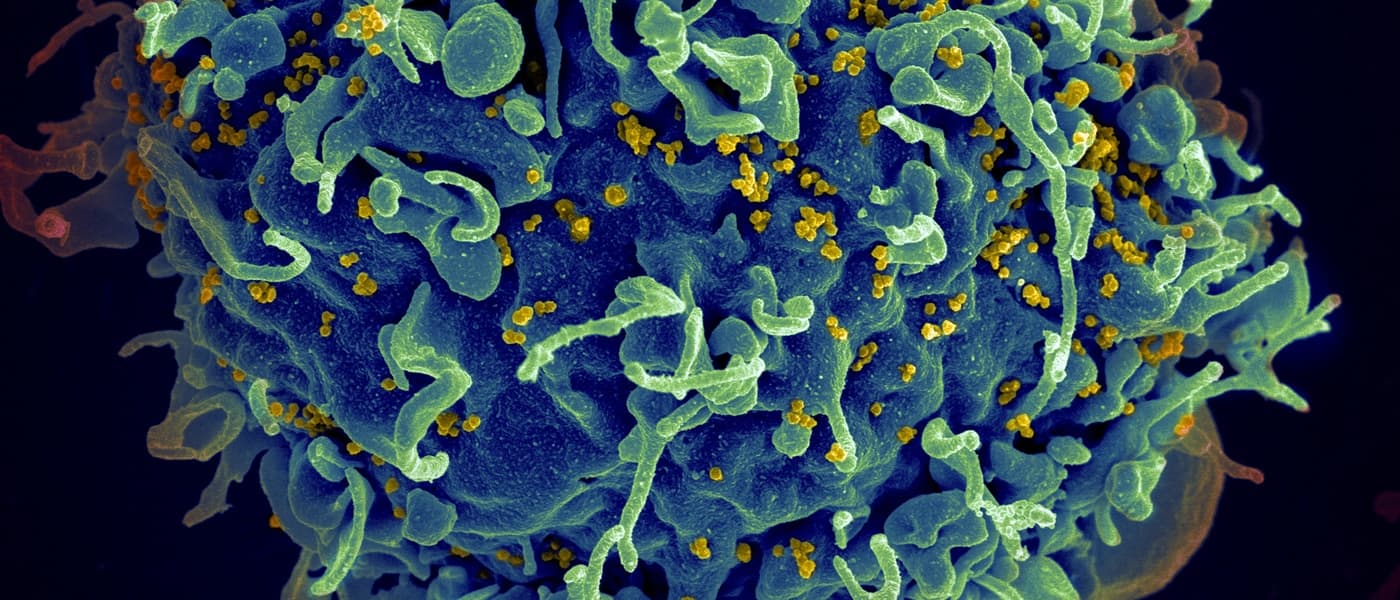
In short, HIV is the virus. It attacks our bodies and leads to AIDS, which is a condition that develops when a person’s T-cells drop below 200.
To break this down a bit more, T-cells are the white blood cells that HIV uses as a kind of factory in order to make more HIV. This is a rather bad thing, as T-cells play a fundamental role in the body’s ability to combat illness and disease. Ultimately, if our T-cell count gets too low, we can get a host of diseases that, ordinarily, we would be able to easily fight off.
Currently, there is no cure for HIV, and there is no vaccine.
But fortunately, it is possible to protect yourself against HIV and AIDS, as we know exactly how it spreads—bodily fluids. As Kristen notes, “Really, HIV is not easy to get. It’s not something that you are accidentally going to pick up on the street.” Indeed, although HIV cells live in nearly all parts of the human body, it is only spread if you come in direct contact with blood, semen, vaginal secretions, or breast milk. “Direct contact” means that the HIV cannot make its way through your skin; rather, it has to actually enter your body (through a cut, body orifice, etc.).
Most often, HIV is transmitted through unprotected sex or a contaminated needle, which means that you can easily protect yourself by only using clean needles (ones that have never been used before) or using condoms when engaging in intercourse.
HIV is not spread through saliva. None. At all. Not 5 ounces. Not 5 gallons. Not 500 gallons. Saliva does not spread HIV. So kissing is fine.
Relevant: I'm HIV positive, do you dare to touch me?
It’s also not spread through other forms of casual contact (holding hands, hugging etc.). It’s also not spread through mosquitoes or any other creature (it’s the Human Immunodeficiency Virus, meaning that only humans are carriers). You also don’t need to worry about swimming pools, and although HIV used to be transmitted through blood transfusions, blood screening processes effectively negated this risk.
The Epidemic Begins:
Kristen notes that, although scientists didn’t become aware of the HIV epidemic until the early 1980s (1981, to be exact), they believe that humanity actually first encountered the disease more than a century earlier.
But if people were living with, and dying from, this virus for more than one-hundred years, why didn’t we notice?
Ultimately, Kristen states that the answer comes down to the way that HIV impacts the body: “Because HIV affects the immune system, people get sick with otherwise normal infections or diseases. So back in the 30s, 40s, and 50s, if someone died of pneumonia, or died of the flu or even a cold…no one really thought anything of it.” As such, it wasn’t until the 80s, when large clusters of people started getting sick with a specific and very rare form of skin cancer, that we realized there was a connection.
And in these early years, being diagnosed with HIV was a very bad thing.
In fact, according to Kristen, getting diagnosed with HIV in the 1980s was like getting the Black Death in the Middle Ages: “If you found out that you had this…once you saw that you had a purple lesion, you were dead. It was kind of like that moment when, once they saw the black lesions, they [victims of the Black Death] knew that they were dead.”
There was simply no hope for patients at this juncture because, as Kristen notes, doctors had simply no idea what they were dealing with. Indeed, things were so bad that, initially, many thought that the virus only attacked homosexuals—that there was something fundamentally different about homosexual biology that made them susceptible to this disease: “It was actually first informally referred to as ‘Gay Cancer,’” Kristen explains, “and when they finally realized what it was, once they realized that people were getting this cancer because of the immune deficiency, the first official name was GRID, Gay Related Immune Deficiency.”
And because we knew so little about the virus and how it operates, treatment options were virtually nonexistent. “What we would do is just try the traditional treatment for the cancer or whatever the person had,” Kristen notes. Beyond that, there was nothing that we could do.
The “Game Changer”:
A new door was opened about 3 years after the start of the epidemic. HIV tends to hide in the cells of the body, and when you remove it from the human body, the virus dies extremely fast. As a result, scientists researching the disease couldn’t keep their samples alive long enough in order to locate the virus. So it wasn’t until 1984 that we had our first real breakthrough.
At this juncture, Robert C. Gallo, a medical doctor from the United States, and French scientist Luc Montagnier became world famous for the discovery of HIV. Finally, researchers had found the virus responsible for all this illness.
Kristen states that, once we realized what HIV actually was, we were able to develop the first antibody test to definitively tell when someone had HIV. Unfortunately, though we could tell when someone had HIV, we could do little more than let the person know that they were going to die. The first treatment options weren’t to come for another three years.
It was in 1987 that AZT came on the market. Known as “azidothymidine,” this is a drug that reduces the number of HIV cells in the body. Kristen notes that this drug was the first real “game changer:” “It basically had the Lazarus effect on people,” Kristen asserts; “It took individuals from death’s door and just turned them around completely."
Thanks to this drug, individuals who quite literally had no immune system left were able to replenish their T-cells and restore their immune functions.
But although AZT saved lives, Kristen is quick to clarify that its side effects created a host of new nightmares for HIV/AIDS patients. In addition to the standard side effects that come with most medications, such as headaches, nausea, and vomiting, AZT is also known to cause severe blood problems (including a decrease in red blood cells and white blood cells), muscle wasting, and severe (sometimes fatal) liver problems.
But despite its complications, it is this drug that, for the most part, was all that we had for the next decade.
The Next Giant Leap for Mankind:
In 1995, we had the next big change. This is when combination therapy developed. Prior to this, we used monotherapy (a reliance on exclusively one drug for treatment). “What we noticed is that people would do really well one drug for maybe six months, a year, or even a couple of years," Kristen explains. "Then their numbers [their T-cell count] would start to slip, and they would get really sick again.” She goes on to note that the only recourse was to switch to another drug, which would work for a time and then, like the drug that came before it, it would be rendered ineffective.
Then, in the mid-90s, we started to give people all the different drugs at the same time.
What they figured out is that you need to take at least three different drugs out of three different classes of drugs. Each class of drug stops HIV in a particular part of its development. So if the first drug is stopping step two, and some of the HIV survives, we need another drug to back it up and catch anything that survives, and then another drug to back up the first two…and in a way, you can think about it like antibiotic resistance. Basically, if enough HIV can continue to replicate, it makes a change. It literally changes its RNA…so it takes a detour around the medication that is stopping it. And if that keeps happening, if that’s the only medication in the person’s body, all we have left is the mutated, resistant virus.
Combination therapy effectively blocked this mutation process, ensuring that HIV could not become resistant to our treatments.
Ultimately, this is the treatment that we still use, but of course, it’s not fool-proof. As Kristen notes, taking all of your medication, and taking it on time, is of dire importance: “If a person is not 90 to 95% adherent to it [their treatment], then they run the risk of the HIV becoming resistant to that drug….so if a person is only going to sort of be adherent to their treatment, it’s actually worse than not having treatment at all, because at least, that way, they won’t become resistant to the medication.”
Kristen states that adherence is even more important when one considers that this drug resistance can be transmitted (though this is relatively uncommon). In any case, today, if you follow the aforementioned treatments, there is absolutely no reason that you can’t live out your life as (for the most part) you otherwise would have.
That said, Kristen emphasizes that HIV is still a serious issues disease: “You have no shorter life expectancy than someone without HIV, so I compare it to diabetes. Obviously, there are lots of differences between the two, but both HIV and diabetes can kill you. They can have drastic physical consequences if you don’t take care of them, but you can deal with it. It might not be fun…but it’s absolutely livable.”
The Future of HIV: Vaccines and the Cure
So, what’s the next step on the road to a cure?
Recently, there have been a number of reports that make bold claims about HIV vaccines; however, Kristen notes that, to date, the most successful trial, which took place more than a decade ago (in 2003) only had a 30% success rate. “This is clearly not enough, but people got really excited because they thought, ‘okay, at least we got something. There is something in this vaccine that is working;’” however, Kristen states that, unfortunately, “since then, we haven’t gotten anything.”
Kristen goes on to explain that this lack of forward movement is primarily because of HIV’s excessive mutation rate. Since HIV mutates so incredibly quickly, we haven’t discovered a way to create antibodies that are effective against all the HIV strands out there. Kristen states, “We could successfully vaccinate someone against a couple varieties of HIV, but then there is this infinite number of other types of HIV out there that we can’t vaccinate against.”
But then, what about the individual who was cured of HIV?
While Kristen notes that these reports are true, the method used isn’t viable for a cure. She explains that the patient's name is Timothy Brown, and that he was diagnosed both with leukemia and HIV. As such, he needed a bone marrow transplant (this was to treat his cancer). Ultimately, the doctors found a donor and, as it turns out, this donor is immune to HIV.
Yes, some people are immune to HIV.
Kristen explains, “A very, very small portion of the human population has a genetic mutation on their T-cells that makes their receptor defective, so these people can’t get HIV…and so when the doctors gave this man [Brown] the bone marrow, his body started producing HIV resistant T-cells. When this happened, any HIV that was left in his system after the treatment couldn’t replicate, and it died off.” To date, Brown has been off of HIV medicine for some 8 years, and he still has no detectable HIV cells in his body.
So, why don’t we use this for everyone?
Kristen points out that, first, bone marrow transplants are very dangerous: “You have to wipe out your entire immune system. Compared to those living with HIV, the fatality rate for bone marrow transplants is rather high [for older individuals, the 7 year survival rate is just 20%]. So if someone only has HIV, which is now classified as a chronic, manageable illness, we’re not going to do something that has a risk of death in order to cure them.”
In short, if you have access to treatment, you are more likely to die of a bone marrow transplant than die of HIV.
Second, only 1 to 2% of individuals have this mutation. As such, for a great many people, it is nearly impossible to find a genetic match that has this mutation. Yet, Kristen notes that some researchers are hopeful and are currently looking into ways that we can produce this mutation synthetically. In fact, she states that synthetic treatments have already been tried on individuals in the United States; however, the results of these studies are not out yet. And even if it proves to be viable, Kristen notes that it will probably be at least a decade before such treatment passes all FDA regulations and is made available.
Yet, there is more hope. Though there may not be a cure, soon, we may be able to prevent new infections.
Kristen was quick to say that, despite the setbacks with a vaccine, there is an exciting breakthrough that was recently approved by the FDA—PrEP (Pre-Exposure Prophylaxis). This is a prevention that is used before exposure. “The idea behind it is that we give people who are HIV-negative a treatment that is used to fight HIV,” Kristen states. “It’s known as Truavda…it’s basically the medication that stops HIV from replicating in the body, so if people are exposed to HIV, the HIV can’t replicate, and if the HIV can’t replicate, it dies.”
This could change the lives of those who are at risk of HIV exposure (such as an HIV negative individual who has an HIV positive partner, injection drug users etc.).
Other Ways to Fight HIV:
The best way to ensure that you don't get HIV is to know how to protect yourself. According to Kristen, the most important thing that you can do for yourself, and to help others, is to get informed. Know how you can get HIV, know what behaviors put you at risk, know how to protect yourself, and be ready to talk with friends and family who may be misinformed.
And know that you can only help; you can’t make other people’s decisions for them.
“If people are going to engage in a behavior, they are going to engage in a behavior. So we are going to give them the tools that they need to do that safely,” Kristen asserts, and she states that those tools include both knowledge and access to safe, reliable protection (including condoms, clean needles, etc.).
This dual attack, providing both knowledge and recourses, has been proven to be effective. Indeed, a number of studies have shown that providing individuals with access to protection does not increase or encourage any risky behaviors, but (and here’s the notable thing) it does decrease the number of infections. “Syringe exchanges have been proven to not increase drug use, and they don’t pose any sort of public health risks,” Kristen explains, and she goes on to note that such programs have been shown to decrease instances of both HIV and Hepatitis C among drug users.
She also notes that these programs are a great way to form lasting change, as they allow individuals to establish trust and form relationships, which is the first step to getting individuals access to long-term solutions, like therapy and drug rehab: “You don’t just say, ‘Stop using drugs.’ That doesn’t work. It’s a process…a person is not going to get clean until they are ready.”
Kristen asserts that this is why a number of organizations, like Trillium Health, have needle exchange programs and similar services. Treating individuals once they already have the virus is far less desirable than stopping individuals from getting it in the first place.
To that end, although abstaining is the only 100% way to protect yourself, there are a number of ways that you can make yourself safer.
- Always make sure that you use clean needles. Never share. If you are in need, there are a number of places that you can go to get access to clean supplies.
- Always use condoms, dental dams, and other forms of protection when engaging in intercourse. And note that the “always” is absolutely key.
- If you participate in any behaviors that may put you at risk, get tested. As is true of all illnesses, early detection is important.
- If you are infected, know that it’s not the end of the world (not even close). There are a number of individuals and organizations that are there to offer their help. Don’t be afraid to ask.
Share This Article