Sleeping Menace
Dormant bacteria in human blood may be causing inflammation, excessive clotting, and deformed protein sheets. Previously believed to be free from microbes, recent DNA sequencing has revealed that there may be around 1000 bacterial cells in each milliliter of blood. These bacteria may be triggering reactions that lead to symptoms commonly associated with stroke, heart attack, diabetes, arthritis, and even Alzheimer's disease.
It is unclear how these symptoms are linked.
Researchers Douglas Kell, at the University of Manchester, and Resia Pretorius, from the University of Pretoria in South Africa, believe that when high levels of iron are introduced in blood, these dormant bacteria awaken. They then release molecules called lipopolysaccharides (LPS). LPS stays on the bacteria's cell wall, and rendering them recognizable by the immune system. This triggers inflammation, which is one of the immune system's defense mechanisms.
Series of Symptoms
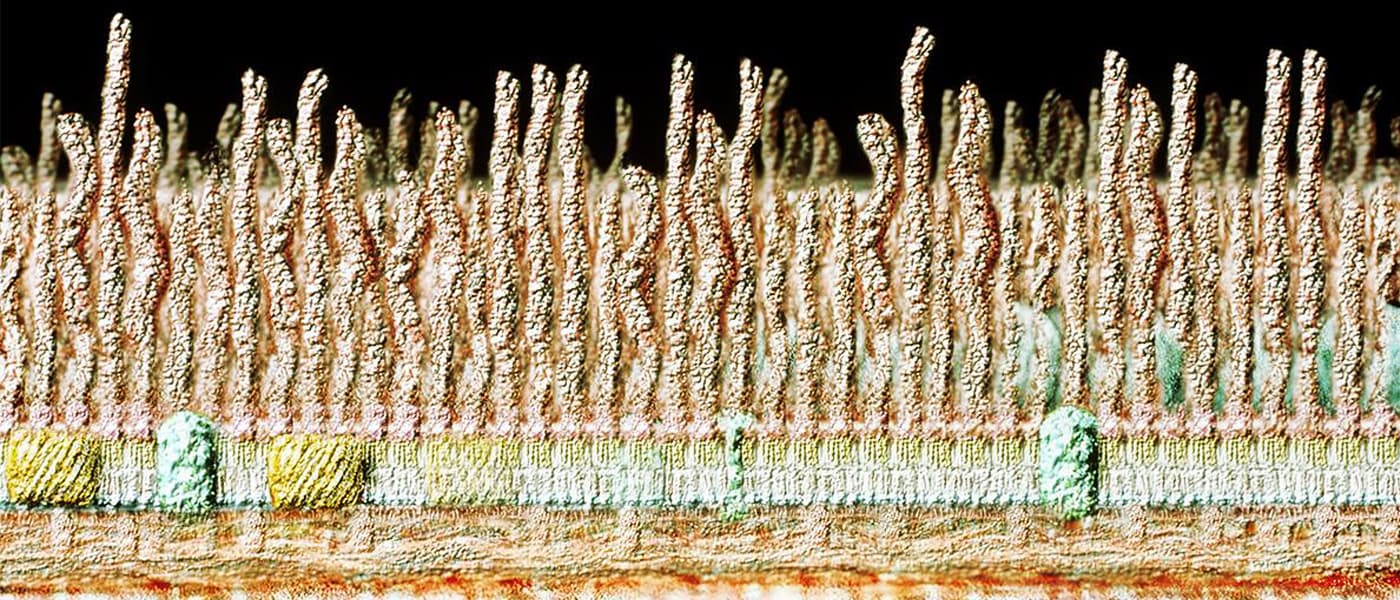
LPS affects blood clotting, too. The researchers conducted a test where they mixed LPS with E. coli bacteria and fibrinogen, a protein in blood that forms the fibrin structures in clots. The results showed that fibrinogen reacts with LPS, triggering the formation of abnormal clots similar to those in heart attacks, strokes, and thrombosis. Apparently, LPS changed the fibrin structure, making it unusually thicker, bending the fibrinogen out of shape. The abnormal proteins spread, causing excessive blood clotting.
LPS triggers inflammation and creates aberrant fibrinogen that spreads abnormally, creating conditions that make the body more susceptible to heart attack and stroke. These conditions are also seen in rheumatoid arthritis and Alzheimer's, two diseases that involve high levels of iron, which wakes the bacteria in blood, in the first place.
The conditions are inextricably linked, it seems. Further research is needed to figure out a way to deal with this bacteria.
The research was published in the Journal of the Royal Society Interface.
Share This Article